WHAT YOU NEED TO KNOW: What do I need to know about cardioversion? Cardioversion is a procedure that uses medicine or electric shocks to correct arrhythmias. An arrhythmia is a heartbeat that is too slow, too fast, or irregular. It may prevent your body from getting the blood and oxygen it needs. Your heart has 4 chambers, called the atria and ventricles. The atria are at the top of your heart, and the ventricles are at the bottom of your heart. Most arrhythmias that need cardioversion start in the atria. 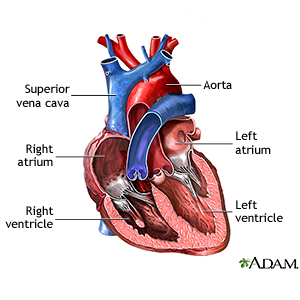
|
How do I prepare for cardioversion? You may need a transesophageal echocardiogram (TEE) before your cardioversion. A TEE is an ultrasound to check for clots in your heart. You may need to take blood thinner medicine for several weeks before your cardioversion. This will help prevent blood clots. Your healthcare provider will talk to you about how to prepare for cardioversion. He may tell you not to eat or drink anything after midnight on the day of your cardioversion. He will tell you what medicines to take or not take on the day of your cardioversion. Arrange for someone to drive you home and stay with you for 24 hours. This person can call 911 if you have problems after your cardioversion. What will happen during a chemical cardioversion? You will be placed on a heart monitor. A heart monitor is an EKG that records your heart's electrical activity. Your healthcare provider will inject 1 or more medicines into your IV. The medicines will help change your heartbeat to a normal rhythm. You may feel light headed, dizzy, or nauseous. You may have pain or pressure in your chest, jaw, shoulders, or arms. These symptoms are normal, and usually last for a minute or less. You may need electrical cardioversion if chemical cardioversion does not change your heartbeat to a normal rhythm. What will happen during an electrical cardioversion? You will be given medicine through your IV to keep you asleep and free from pain. You will be placed on a heart monitor. A heart monitor is an EKG that records your heart's electrical activity. A healthcare provider will also monitor your blood pressure and oxygen levels during the procedure. You may get oxygen through a mask placed over your nose and mouth or through small tubes placed in your nostrils. - In external cardioversion your healthcare provider will place sticky pads on your chest and back. Your heart will be shocked with electricity through the pads. Your heart may be shocked more than once to help it return to its normal rhythm.
- In internal cardioversion your healthcare provider will insert a catheter through a vein and into your heart. Your heart will be shocked through the catheter. Your heart may be shocked more than once to help it return to its normal rhythm.
What will happen after cardioversion? Healthcare providers will monitor your heartbeat, blood pressure, and oxygen levels. You may feel drowsy from the medicine you were given during the procedure. Your chest may be red or sore where the pads were placed. This should go away in a few days. You may go home when they say it is okay or you may need to stay in the hospital. What are the risks of cardioversion? Your skin may be burned from the electric shocks. Cardioversion may cause a blood clot to travel to your heart or brain and cause a heart attack or stroke. You may develop a life-threatening arrhythmia or low blood pressure during cardioversion. You may need medicine or more electric shocks to treat this. Even with cardioversion, your heartbeat may not change or may not stay regular. |